As we all know, disposable thoracentesis device is the key tool for thoracentesis. What should we know about thoracentesis?
Indications for Thoracocentesis
1. Diagnostic puncture of chest trauma suspected of hemopneumothorax, which needs further clarification; The nature of pleural effusion is undetermined, and the pleural effusion needs to be punctured for laboratory examination.
2. When a large amount of pleural effusion (or hematocele) is punctured therapeutically, which affects the respiratory and circulatory functions, and is not yet qualified for thoracic drainage, or pneumothorax affects the respiratory function.
Thoracocentesis method
1. The patient sits on the chair in reverse direction, with the healthy arm on the back of the chair, the head on the arm, and the affected upper limb extended above the head; Or take a half side lying position, with the affected side upward and the affected side arm raised above the head, so that the intercosts are relatively open.
2. The puncture and drainage should be performed at the solid sound point of percussion, generally in the 7th to 8th intercostal space of the subscapular angle, or in the 5th to 6th intercostal space of the midaxillary line. The puncture site of encapsulated effusion should be located according to X-ray fluoroscopy or ultrasonic examination.
3. Pneumothorax aspirates, generally in the semi recumbent position, and the ring piercing point is at the midclavicular line between the 2nd and 3rd intercostals, or at the front of the armpit between the 4th and 5th intercostals.
4. The operator should strictly perform aseptic operation, wear a mask, cap and aseptic gloves, routinely disinfect the skin at the puncture site with iodine tincture and alcohol, and lay a surgical towel. Local anesthesia should infiltrate the pleura.
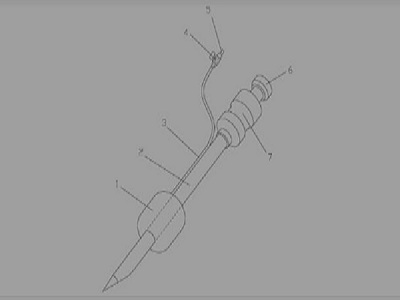
5. The needle should be inserted slowly along the upper edge of the next rib, and the latex tube connected to the needle should be clamped with hemostatic forceps first. When passing through the parietal pleura and entering the thoracic cavity, you can feel the "sense of falling" that the needle tip resists the sudden disappearance, then connect the syringe, release the hemostatic forceps on the latex tube, and then you can pump fluid or air (when pumping air, you can also connect the artificial pneumothorax device when it is confirmed that the pneumothorax is pumped out, and perform continuous pumping).
6. After fluid extraction, pull out the puncture needle, press 1~3nin with sterile gauze at the needle hole, and fix it with adhesive tape. Ask the patient to stay in bed.
7. When critically ill patients are punctured, they generally take the flat position, and should not move their body too much for puncture.
Precautions for Thoracocentesis
1. The amount of fluid drawn by puncture for diagnosis is generally 50-100ml; For the purpose of decompression, it should not exceed 600ml for the first time and 1000ml for each time thereafter. During traumatic hemothorax puncture, it is advisable to release accumulated blood at the same time, pay attention to blood pressure at any time, and speed up blood transfusion and infusion to prevent sudden respiratory and circulatory dysfunction or shock during fluid extraction.
2. During the puncture, the patient should avoid coughing and body position rotation. If necessary, codeine can be taken first. In case of continuous cough or chest tightness, dizziness, cold sweat and other collapse symptoms during the operation, the fluid extraction should be stopped immediately, and adrenaline should be injected subcutaneously if necessary.
3. After the pleural puncture of fluid and pneumothorax, the clinical observation should be continued. The pleural fluid and gas may increase again several hours or one or two days later, and the puncture can be repeated if necessary.
Post time: Oct-25-2022





